MEDICARE ADVANTAGE PART 1
NOTE: Availability of Medicare Advantage plans will vary by service area. Carriers, benefit amounts, networks, and other factors vary per plan and are based on annual contracts.
HISTORY OF MANAGED MEDICARE PLANS
Medicare managed care plans started in the early 1970’s.
In the Balance Budget Act of 1997 they were called Medicare + Choice. Then in 2003 in the Medicare Modernization Act, they were renamed Medicare Part C (Medicare Advantage plans) and prescription drug coverage (Part D) was introduced to Medicare beneficiaries.
Managed Care Plans Defined (Source: U.S. National Library of Medicine)
Managed care plans are a type of health insurance. They have contracts with health care providers and medical facilities to provide care for members at reduced costs. These providers make up the plan’s network. How much of your care the plan will pay for depends on the network’s rules.
OVERSIGHT
CMS (Centers for Medicare & Medicaid Services) administers Medicare Part C (Medicare Advantage) plan. CMS sets the marketing rules and regulations for marketing and selling of Medicare Advantage (MA) plans.
AHIP (American Health Insurance Plans) certification is required to sell most Medicare Advantage Plans. In addition to AHIP, carrier certification is also required. Both are required to be renewed annually.
MEDICARE PART C PLANS DEFINED
Medicare Advantage plans are network based managed care programs.
They are available in three main plans:

To learn more about each, see page 90 in the 2016 edition of the Medicare & You publication
3 MAIN TYPES OF MEDICARE ADVANTAGE PLANS
NOTE: MA only HMO and PPO plans cannot be paired with a Part D plan.
Medicare Advantage Plans become primary over original Medicare (unlike Medicare supplement plans, which work secondary to Medicare). Clients still retain their Medicare Parts A and B.
Medicare Advantage plans are required to cover what Medicare covers, and have the option to cover more.
FUNDING
Medicare Advantage plans are funded through capitation rates based on the areas they are providing service. The carriers providing Medicare Advantage plans receive this funding, and have the option of charging a monthly premium to their plan members.
RATINGS
Plans are scored by CMS by a 5-star rating system, 5 starts being the highest rating possible. The higher a star rating, the more the carrier may receive in funding and/or bonus from CMS.
Low Performing Plans
Beneficiaries will receive a letter from CMS if they are in a plan that is considered low performing (having a star rating of 2.5 or less for 3 years) informing them to review their plan.
5-Star Rated Plans
Beneficiaries have a special enrollment period (more on enrollment in later sections) which will allow them one change to a 5-star rated plan once per year.
FINDING PLANS IN YOUR AREA
You can find plans in your area by using Medicare.gov, using the option “Find Health & Drug Plans.”
FLASHCARDS! HOVER OVER EACH CARD
TO SEE THE CORRECT ANSWER
What are the 3 types of network based Medicare Part C plans?
PPO: Preferred Provider Organization
PFFS: Private Fee For Service
What are the 3 main types of MA Plans?
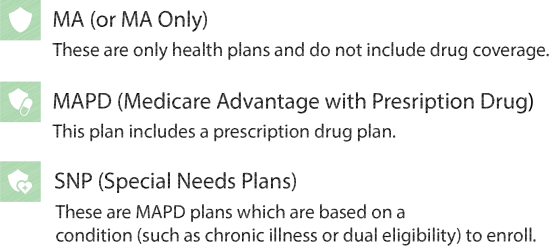
MAPD (Medicare Advantage with Prescription Drug)
SNP (Special Needs Plans)
